From 2008, we have been investigating the effects of (human) retinal laser irradiation, a specific project of the general bio-thermo-fluids problem of laser interaction with tissues irrigated by blood flow. The work was done with suitable and timely input from (Dr. Lingam Gopal, then Chairman of) the research division of Shankar Nethralaya, a Chennai-based leading eye care institute. This note is a summary of some of the research results communicated so far. A follow-up note in a while, should explain more of the ongoing work. Some eye candy from our simulations is also provided (CFD a la Colorful Fluid Dynamics although here it is more of CHT, colorful heat transfer).
(Note: If you are seriously interested in this research, from a beach-walker curious of flashing pebbles, to an undergraduate cautious to wet the feet from an optimal graded distance just for the thrill of it, to graduate students and fellow bio-thermo-fluids researchers wanting to dive in and gasp along in (the uncertain) search for a pearl or two, do write to me. I am especially looking for some collaborative experimental ventures.)
Now for some specifics about the research.
Laser surgery is routinely used in the treatment of a range of eye diseases such as retinal detachment, choroidal neovascularization, and macular degeneration. During laser irradiation, the retinal pigmented epithelium (RPE) and the adjacent pigmented choroid absorb most of the laser energy. This causes local heating of the tissues. The human eye has to physiologically cope with temperatures much higher than the body core temperature (37 degree C). For therapeutic purposes, laser irradiation should produce controlled thermal burns or coagulation within the eye. The photocoagulation temperature is around 60 degree C. Irradiation should be controlled such that a specific spot is heated to no more than this temperature. Overheating could cause serious damage to adjoining healthy regions by disrupting cellular mechanisms.
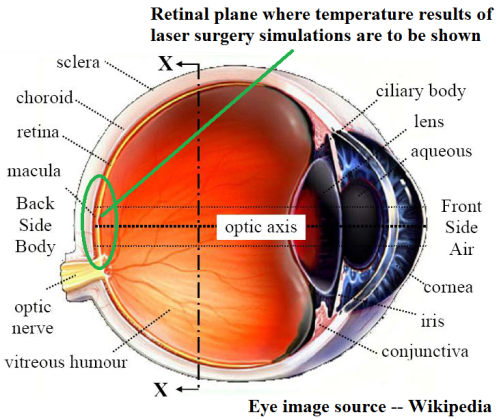
We checked out the temperature distribution and evolution inside the human eye during a typical retinal laser surgery using computational bio-heat transfer modeling and simulation studies performed on faithful 3D eye geometry.
Human eye properties are well documented. The numerical simulation details are provided in the papers mentioned below, in the references. If you already see the world as Neo did in Matrix, you can dive into those papers directly. Here is a gist. Simulation of the retinal laser surgery (for humans) have been performed with various levels of complexity in nature (steady, transient), computational domain (two and three dimensional faithful eye geometries), thermophysical properties (constant, sensitive temperature dependency, effective combination of properties etc.) and modeling equations (various forms of the Pennes-bio-heat transfer equation plus the flow equations, along with specific radiation and evaporation models). The irradiation has also been simulated not only as a simple 1-D ray but also faithful to the actual surgery, as a three dimensional multi-spot array of square and circular distribution, scanned through sequential (in time) and simultaneous (heating of all spots for a while) heating.
Here is a video summary of the simulated retinal laser irradiation by multi-spot heating.
To compare with the real thing, check the laser surgery video here.
Video courtesy: Doctor Lehr, MD (Was freely available at a website that I am unable to locate now; link-tip welcome).
Read more about the Pascal laser that is being used in such surgery, whose specifics were used in our simulations.
Some specific results from the simulation studies are as follows:
Choroid of the eye is vascular and provides blood flow to the retinal region. The effect of the possible convection cooling of the retina that is being irradiated by laser energy is studied as a transient simulation of surgical conditions. While in steady state the convection did have an influence, during the transient heating for about two minutes, the choroidal blood convection was found to be negligible, when compared to the local enthalpy increase and the incident energy.
Not only the human retina but the adjacent choroid is also pigmented and capable of absorbing incident light energy. The effect of laser energy attenuation in the choroid due to it pigmentation, has been investigated. The thickness and location of pigmented layer of choroid have significant effect on peak temperature evolution and resulting diffusion in the retinal region. Increase in thickness or moving the location of pigmented layer of choroid away from the RPE, results in decrease of peak temperature of the retinal region.
Irrespective of blood perfusion, choroidal pigmentation is found to have significant effect on retinal temperature distribution.
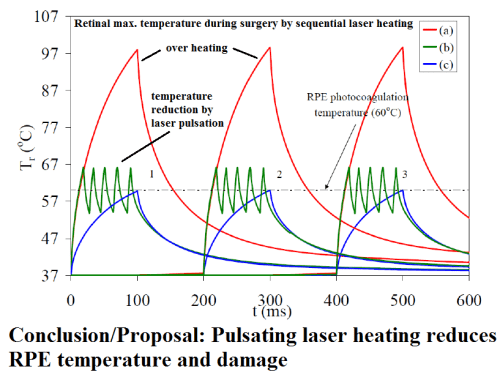
Using the actual retinal irradiation specifications during a surgery, the simulation results suggested over-heating of certain retinal regions. It is shown that the retinal temperature during transient laser heating could reach values higher than that required for irreversible cell damage or photocoagulation (60 C). For a 0:2 W laser power and 500 micro-meter spot diameter, peak retinal temperatures during steady state and transient simulation of 100 ms are 172 C and 104 C respectively.
Two simple techniques are proposed and justified to minimize heat induced tissue damage due to overheating. One method involves pulsation of the applied laser power between a suitable maximum and minimum heat flux values to reduce the heat diffusion zone. Another method calculates the required power setting to maintain the photocoagulation temperature of around 60 degree C. There is an uncertainty for the exact value of the photocoagulation temperature in the literature as it is also a function of other parameters. For a 500 micro-meter laser heating spot size, the lasing power required is found to be 0.072 Watts.
In the larger perspective, this bio-thermo-fluids simulation based investigation helps in understanding the basics of heat evolution in the human eye during laser surgery and can assist practitioners of laser surgery to design therapies that are better and safer than the existing treatment techniques.
Here is a peer-reviewed, open access, research paper published in Frontiers in Heat and Mass Transfer available as Free PDF Download (Narasimhan, A. and Jha, K. K., (2011), “Bio-Heat Transfer Simulation of Square and Circular Array of Retinal Laser Irradiation,” Frontiers in Heat and Mass Transfer, 2, 033005, DOI: http://dx.doi.org/10.5098/hmt.v2.3.3005). Abstract of the FHMT paper.
Excerpts from another Graphical Abstract from a recent (Jan 27, 2012) research paper (Narasimhan, A. and Jha, K. K., (2012), “Bio-Heat Transfer Simulation of Retinal Laser Irradiation,” Int. J. Numer. Meth. Biomed. Engng. DOI: 10.1002/cnm.1489):
[…] influence of choroidal pigmentation and that of choroidal blood convection—parameterized as a function of choroidal blood perfusion—are investigated in detail. […] Because of the participation of pigmented layer of choroid in laser absorption, peak temperature is reduced to 94?°C after 100?ms of the laser surgery period. The effect of choroidal blood perfusion on retinal cooling is found to be negligible during transient simulation of retinopathy. [A] truncated three-dimensional model incorporating multiple laser irradiation of spots […] observe the spatial effect of choroidal blood perfusion and choroidal pigmentation. For a circular array of seven uniformly distributed spots of identical diameter and laser power of 0.2?W, transient temperature evolution using simultaneous and sequential mode of laser surgical process is presented with analysis.
Few more publications — behind pay-wall — related to this study (write to me for a copy of these).
- Jha, K. K. and Narasimhan, A., (2011), “Three-Dimensional Bio-Heat Transfer Simulation of Sequential and Simultaneous Retinal Laser Irradiation,” Int. J. Thermal Sci., 50(7), 1191-1198. [DOI:10.1016/j.ijthermalsci.2011.02.005]
- Narasimhan, A. and Jha, K. K., (2010), “Transient Simulation of Multi-spot Retinal Laser Irradiation using Bio-Heat Transfer Model”, Numerical Heat Transfer, Part A: Applications, 57(7), 520-536. [DOI:10.1080/10407781003684514]
- Narasimhan, A., Jha, K. K. and Gopal, L., (2010), “Transient Simulations of Heat Transfer in Human Eye undergoing Laser Surgery”, Int. J. Heat and Mass Transfer, 53 (1), 482-490. [DOI 10.1016/j.ijheatmasstransfer.2009.09.007].
—–
References Discussed
Narasimhan, A., & Jha, K. (2011). BIO-HEAT TRANSFER SIMULATION OF SQUARE AND CIRCULAR ARRAY OF RETINAL LASER IRRADIATION Frontiers in Heat and Mass Transfer, 2 (3) DOI: 10.5098/hmt.v2.3.3005
Jha, K., & Narasimhan, A. (2011). Three-dimensional bio-heat transfer simulation of sequential and simultaneous retinal laser irradiation International Journal of Thermal Sciences, 50 (7), 1191-1198 DOI: 10.1016/j.ijthermalsci.2011.02.005
